Delving into an overarching concern that influences the well-being of countless individuals, we reflect upon an enigmatic state of dental health that can lead to discomfort and potential repercussions. With an intricate network of soft tissues that envelop the teeth, there exists a possibility of encountering an unanticipated condition that requires our attention and understanding. Discovering the underlying factors and avenues of resolution could pave the way for a healthier oral environment.
Hovering over the realm of oral health, we uncover a particular element that often eludes our attention. This ethereal realm, characterized by an inflamed or irritated nature, manifests itself within the intricate structure that supports our teeth - a realm we come to understand as the oral cavity. Harmonious functioning of this delicate terrain is far from guaranteed, as various factors can unleash havoc upon the otherwise unassuming fortresses that protect our pearly whites.
Enter into the labyrinth of oral woes and ponder upon the significance of this distinctive predicament that silently affects numerous lives. Referred to by those in the know as the affliction that resonates within the soft tissues surrounding our dental structures, it bears the characteristic signs that demand our attention. The affliction, though concealed from plain sight, casts a shadow of unease that one cannot ignore, persistently nagging at one's consciousness.
Arming ourselves with knowledge and insight is key to navigating this perplexing landscape. Equipped with a comprehensive understanding of the underlying causes and potential treatment options, we empower ourselves to address this concern head-on. By conveying the importance of recognizing the early warning signs and exploring the avenues of relief, we embark on a journey towards a healthier, more vibrant oral existence.
Understanding Gum Infections: Vital Knowledge for Dental Health

Gaining a comprehensive understanding of gum infections is crucial to maintaining optimal oral health. This informative section delves into the fundamental principles of gum infections, providing valuable insights into their causes, symptoms, and possible treatments.
The Underlying Causes and Risk Factors
When it comes to gum infections, several contributing factors can lead to their development. These factors include poor oral hygiene practices, inadequate nutrition, hormonal changes, tobacco use, certain medications, and genetic predisposition. Identifying and addressing these causes is crucial in preventing and treating gum infections.
The Symptoms and Warning Signs
Gum infections present themselves through a range of symptoms that should never be ignored. These warning signs include redness and swelling of the gums, tenderness and bleeding during brushing or flossing, persistent bad breath, receding gumline, loose teeth, and the presence of pus between the teeth and gums. Recognizing these symptoms can prompt timely intervention and prevent further complications.
The Importance of Timely Treatment
Timely treatment of gum infections is essential to prevent their progression and potential complications. The primary goal of treatment is to eliminate infection, control inflammation, and promote gum tissue healing. Treatment options can include professional dental cleanings, antibiotics, deep cleaning procedures, and, in severe cases, surgical intervention.
Preventive Measures for Gum Infections
Prevention plays a crucial role in maintaining gum health. Establishing a consistent oral hygiene routine, which includes brushing twice daily and flossing regularly, is imperative. Additionally, adopting a balanced diet, avoiding tobacco products, managing stress levels, and scheduling regular dental check-ups can significantly reduce the risk of gum infections.
In conclusion, developing a thorough understanding of gum infections empowers individuals to take proactive measures in maintaining their dental health. Recognizing the causes, symptoms, and available treatments allows individuals to seek appropriate care and prevent further complications. Prioritizing preventive measures ensures long-term gum health and overall oral well-being.
The Role of Inadequate Oral Care in Gum Infections
Poor oral hygiene plays a significant role in the development and progression of gum infections. Neglecting proper dental care routines can lead to a buildup of bacteria and plaque on the teeth and around the gum line, increasing the risk of inflammation and infection.
When oral hygiene is subpar, irregular or insufficient brushing and flossing allow bacteria to thrive in the mouth. These bacteria can then multiply and form a sticky substance called plaque, which adheres to the teeth. Over time, if left unaddressed, plaque hardens into tartar, which provides a conducive environment for bacteria to grow and multiply, leading to gum infections.
Furthermore, inadequate oral care can result in the accumulation of food particles between the teeth and along the gum line. These trapped particles provide a food source for bacteria, allowing them to thrive and manifest into gum infections. Additionally, poor dental hygiene can cause tooth decay, gum recession, and the formation of cavities, all of which contribute to an increased risk of gum infections.
To prevent gum infections, it is crucial to practice proper oral care. Regular brushing and flossing, at least twice a day, helps remove plaque and bacteria from the teeth and gum line. Using an antimicrobial mouthwash can further aid in reducing bacteria in the mouth.
| Key Points: |
|---|
| - Poor oral hygiene promotes the development and progression of gum infections |
| - neglecting dental care routines allows bacteria to multiply and form plaque |
| - plaque buildup can harden into tartar, providing an ideal environment for bacteria |
| - accumulations of food particles between teeth and gums can lead to infections |
| - practicing regular brushing, flossing, and using mouthwash can help prevent gum infections |
Food for Thought: The Relationship Between Diet and Gum Infections
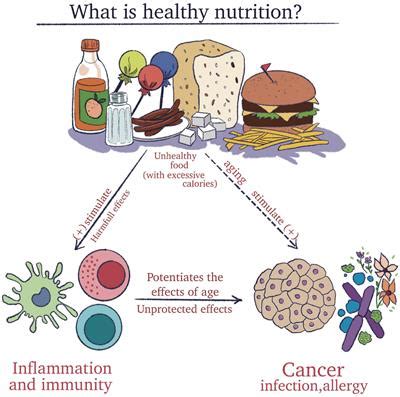
Exploring the connection between our dietary choices and the occurrence of gum infections can provide valuable insights for maintaining oral health. The foods we consume play a significant role in influencing the health of our gums.
Impact of Diet on Gum Health
Our diet serves as the primary source of nutrients for our bodies, including our gums. A balanced diet consisting of essential vitamins, minerals, and other vital nutrients is crucial for the overall health of our gums.
Link Between Poor Nutrition and Gum Infections
When our diet lacks adequate nutrition, our gums become vulnerable to infections. Nutritional deficiencies weaken the immune system, making it harder for our bodies to fight off harmful bacteria that can lead to gum infections.
The Role of Sugar
High sugar consumption is often linked to an increased risk of gum infections. The bacteria in our mouths thrive on the sugars we consume, leading to plaque buildup, gingivitis, and potentially gum disease if not addressed.
Recommended Dietary Choices for Healthy Gums
Incorporating a variety of nutrient-rich foods into our diet can promote gum health. Fresh fruits and vegetables, whole grains, lean proteins, and low-fat dairy products are all beneficial for maintaining healthy gums. Additionally, adequate water consumption helps flush away food particles and bacteria that can contribute to gum infections.
Seeking Professional Advice
If gum infections persist despite maintaining a healthy diet, it is crucial to consult with a dental professional. They can provide personalized guidance and treatment options to address the underlying causes and prevent further complications.
Smoking and Gum Infections: A Dangerous Connection
Investigating the correlation between smoking and the development of gum infections reveals a perilous association that demands attention. Tobacco use, through various mechanisms, can significantly increase the risk of gum diseases, leading to potentially severe consequences for oral health.
A comprehensive examination of the detrimental effects of smoking on gum health highlights the detrimental impact of tobacco on the oral environment. Chemical compounds present in cigarettes compromise the body's ability to combat bacteria, impairing the immune response and facilitating the growth of harmful microorganisms. Moreover, the act of smoking itself reduces blood flow to the gums, impeding the delivery of vital nutrients and oxygen to the tissues.
Research studies consistently demonstrate that individuals who smoke are more likely to experience gum infections compared to non-smokers. The harmful substances in tobacco not only destroy the supportive structures of the teeth but also hinder the healing process, lengthening the duration of gum infections and increasing the likelihood of complications such as tooth loss.
Addressing the dangerous connection between smoking and gum infections necessitates immediate action. Smoking cessation programs, combined with regular dental cleanings and effective oral hygiene practices, play a crucial role in mitigating the risks associated with gum diseases. By quitting smoking, individuals can significantly reduce the chances of developing infections, enhance their overall oral health, and improve their overall well-being.
| Key Points: |
|---|
| - Smoking is strongly linked to an increased risk of gum infections. |
| - Chemical compounds in tobacco compromise the immune response against bacteria. |
| - Smoking reduces blood flow to the gums, hindering healing and nutrient delivery. |
| - Research shows that smokers are more prone to gum infections and tooth loss. |
| - Quitting smoking and maintaining proper oral hygiene are essential for preventing gum diseases. |
The Surprising Impact of Stress on Gum Health

When it comes to maintaining healthy gums, one might not immediately think of stress as a contributing factor. However, research and studies have shown that stress can have a surprising impact on gum health.
Chronic stress, which refers to long-term or ongoing stress, can weaken the immune system and make it more difficult for the body to fight off infections and inflammation, including those affecting the gums. In addition, stress can lead to an increase in cortisol, a hormone that can promote inflammation in the body.
Furthermore, stress can also lead to unhealthy behaviors or habits, such as teeth grinding or clenching, which can put additional pressure on the gums and potentially lead to gum recession or damage.
It is important to note that the relationship between stress and gum health is not entirely one-sided. While stress can have negative effects on gum health, poor gum health can also contribute to stress and anxiety. Chronic gum problems can cause pain, discomfort, and embarrassment, leading to increased stress levels and a negative impact on overall well-being.
Managing stress levels and adopting healthy coping mechanisms can play a significant role in maintaining optimal gum health. This may include practicing relaxation techniques, engaging in regular physical activity, getting enough sleep, and seeking support from loved ones or healthcare professionals.
By recognizing the surprising impact of stress on gum health and taking proactive steps to manage stress, individuals can improve their overall oral health and well-being.
Medications and Gum Infections: What You Should Be Aware Of
When it comes to gum infections, it's important to be aware of the potential impacts that medications can have on your oral health. Certain medications, whether over-the-counter or prescribed, can contribute to the development or worsening of gum infections.
One area where medications can have an effect is in the suppression of the immune system. Some drugs, such as corticosteroids or immunosuppressants, may weaken the body's natural defense mechanisms, making it more susceptible to infections in the gums. This is particularly relevant for individuals who are already at a higher risk of gum disease.
Another consideration is the impact of medications on saliva production. Saliva plays a crucial role in maintaining oral health by washing away bacteria and food particles, and by neutralizing acids in the mouth. However, certain medications, such as antihistamines or decongestants, can reduce saliva flow, leading to a dry mouth. A lack of saliva can create an environment where bacteria can thrive, potentially leading to gum infections.
Furthermore, some medications may have direct adverse effects on the gums themselves. For instance, calcium channel blockers used for the management of high blood pressure can cause gum overgrowth or enlargement. This can create pockets around the teeth where bacteria can accumulate, increasing the risk of gum infections.
If you are taking any medications and notice signs of gum infection, such as redness, swelling, or bleeding, it's important to inform your dentist. They can evaluate your oral health and recommend appropriate treatment options to manage the infection. In some cases, adjustments to your medication regimen may be necessary to help improve gum health.
- Be vigilant about oral hygiene practices, such as regular brushing and flossing, to reduce the risk of gum infections.
- Stay hydrated and consider using saliva substitutes or drinking water frequently if you experience dry mouth as a side effect of medication.
- Attend regular dental check-ups to monitor the health of your gums and receive professional cleanings.
Remember, being aware of the potential impact of medications on gum infections and taking appropriate steps to mitigate these risks can help maintain your oral health and prevent complications in the long run.
Diabetes and Gum Infections: Uncovering the Hidden Connection

Exploring the Intricate Link Between Diabetes and Gum Infections
Gum infections and diabetes often share a deeper connection than meets the eye. The presence of diabetes in an individual can significantly increase the risk of developing gum infections, while gum infections can have a negative impact on blood sugar control in those with diabetes. Understanding this intricate relationship is crucial for managing both conditions effectively.
The Role of Diabetes in Gum Infections
Diabetes affects the body's ability to regulate blood sugar levels, leading to several systemic complications. One such complication is impaired immune function, which can make individuals more susceptible to infections, including gum infections. Additionally, diabetes can also reduce blood flow to the gums, impairing their ability to heal and fight off bacteria effectively.
The Impact of Gum Infections on Diabetes Control
Gum infections, such as periodontitis, can have a detrimental effect on diabetes control. The inflammation caused by gum infections can make it more challenging to regulate blood sugar levels, potentially leading to increased insulin resistance. Moreover, the presence of chronic infection can contribute to overall systemic inflammation, further exacerbating the complications of diabetes.
Prevention and Treatment Strategies
Managing diabetes and gum infections requires a comprehensive approach that focuses on both conditions simultaneously. Maintaining good oral hygiene, including regular brushing, flossing, and professional dental cleanings, is essential for preventing gum infections. For individuals with diabetes, closely monitoring blood sugar levels and working closely with healthcare professionals to achieve optimal control is crucial. Additionally, early detection and prompt treatment of gum infections can help prevent their progression and minimize their impact on diabetes control.
In conclusion, the link between diabetes and gum infections should not be overlooked. Understanding the hidden connection and implementing proper prevention and treatment strategies is vital for individuals with diabetes to maintain optimal oral health and diabetes control.
The Importance of Timely Identification and Management of Gum Infections
Giving due attention to the timely detection and appropriate treatment of gum infections is of utmost significance in maintaining good oral health. Identifying and addressing gum infections promptly can help prevent the progression of the condition and minimize its potential adverse effects on overall well-being.
Timely Diagnosis: Recognizing the early signs and symptoms of gum infections plays a vital role in preventing the further development of complications. By closely monitoring the well-being of your gums, you can promptly identify any abnormal changes, such as redness, swelling, or bleeding, that could indicate an infection.
Effective Management: Prompt treatment and intervention are crucial in managing gum infections, as they can prevent the spread of bacteria and the accompanying inflammation. Timely dental care, including professional cleanings, scaling, and root planing, can help remove plaque and tartar buildup, reducing the risk of infection.
Preventing Complications: Treating gum infections in their early stages can prevent the progression of more severe oral health issues. Neglecting such infections can lead to gum disease and even tooth loss. Additionally, gum infections have been associated with an increased risk of cardiovascular disease and other systemic health conditions, highlighting the importance of early detection and intervention.
In conclusion, being vigilant in recognizing the signs of gum infections and seeking timely treatment is essential for preserving oral health and preventing potential complications. Regular dental check-ups and adopting a comprehensive oral hygiene routine can assist in the early detection and successful management of gum infections, ensuring long-term oral well-being.
Exploring Your Choices: Effective Treatment Options for Gum Infections

Gum infections can be a serious dental concern that require prompt and effective treatment. When facing gum infections, it is essential to explore the various treatment options available to address the condition and restore oral health.
One common treatment option for gum infections is professional dental cleaning, also known as scaling and root planing. This procedure involves removing plaque and tartar buildup from below the gumline, helping to eliminate the bacteria causing the infection. Scaling and root planing aims to reduce inflammation and promote gum tissue healing.
Another choice to consider is antibiotic therapy. Based on the severity of the infection, your dentist may prescribe antibiotics to target the specific bacteria causing the gum infection. Antibiotics can be delivered orally or through direct application to the infected gums, assisting in combating the infection and preventing its spread.
For more severe cases, surgical intervention may be necessary. One surgical option is flap surgery, which involves lifting the gums to access the infected areas and remove bacteria, plaque, and tartar. This procedure aims to reduce pocket depth and promote gum tissue reattachment.
In certain situations, gum grafting may be recommended. This procedure involves taking tissue from another part of your mouth or using synthetic materials to replace damaged gum tissue caused by the infection. Gum grafting helps in restoring healthy gum tissue and preventing further complications.
Adjunctive treatments such as dental lasers and antimicrobial mouth rinses can also be utilized alongside primary treatment options. Dental lasers help in removing infected tissue and promoting healthier gum regeneration, while antimicrobial mouth rinses provide additional protection against bacteria.
It is crucial to remember that the choice of treatment for gum infections may vary depending on individual circumstances. Therefore, it is essential to consult with a dental professional who can evaluate your specific condition and recommend the most suitable treatment plan.
- Professional dental cleaning (scaling and root planing)
- Antibiotic therapy
- Surgical intervention (flap surgery)
- Gum grafting
- Adjunctive treatments (dental lasers and antimicrobial mouth rinses)
By exploring these effective treatment options and working closely with your dentist, you can take the necessary steps to address gum infections and maintain optimal oral health.
FAQ
What are the common causes of infected gums?
Common causes of infected gums include poor dental hygiene, plaque buildup, gum disease, hormonal changes, certain medications, and smoking.
Can infected gums lead to serious oral health problems?
Yes, if left untreated, infected gums can lead to serious oral health problems such as gum disease, tooth loss, and even systemic health issues.
What are the symptoms of infected gums?
Symptoms of infected gums may include red, swollen, or bleeding gums, bad breath, receding gums, loose teeth, and the formation of abscesses or pus.
Is there a way to prevent gum infections?
Yes, maintaining good oral hygiene by brushing and flossing regularly, visiting the dentist for regular check-ups and cleanings, and avoiding smoking can help prevent gum infections.
What are the treatment options for infected gums?
Treatment options for infected gums depend on the severity of the infection but may include professional dental cleanings, antibiotics, deep cleaning procedures, gum surgery, or periodontal therapy.